Keeping Prescription Drugs Affordable
The Value of Prescription Drug Coverage & The Role of PBMs

The prescription drug benefit covered by health plans—public and private—is the health insurance benefit most widely used by consumers. In Texas alone there were more than 228 million prescriptions filled at more than 7,000 retail pharmacy settings in 2014, representing $17.6 billion in prescription drug costs.
In recent years, Texans and Americans across the country have seen a sudden spike in the price of prescription drugs—due in large part to the skyrocketing costs of specialty drugs— making the role of pharmacy benefit managers (PBMs) increasingly important in keeping drug costs manageable.
Health plans primarily use pharmacy benefit managers, or PBMs, as an efficient, effective way to manage prescription drug coverage and improve health outcomes. Some health plans maintain prescription drug management in-house, while others contract with PBMs outside of their organizations. PBMs help consumers and employers save on the cost of prescription drugs, while using clinically-based services to reduce medication errors and increase compliance with drug therapies.
Spending on specialty drugs is becoming a bigger share of U.S. prescription drug spending and is growing at a rapid and unsustainable rate. In 2014 alone, U.S. prescription drug spending increased by 13.1 percent— the largest annual increase since 2003—and was largely driven by a 30.9 percent increase in the cost of specialty drugs. Because of the rapid increase in prescription drug costs, the job of managing pharmacy benefits has become even more critical. Left unmanaged, prescription drug costs would rise at even faster rates with the ultimate result of reduced benefits and higher costs to consumers and employers.
Actuaries from the Centers for Medicare and Medicaid Services (CMS) estimate that PBMs’ use of prescription drug management tools, including encouraging the use of generic drugs, helped slow prescription drug spending growth from 5.3% in 2009 to 3.5 percent in 2010. From 2012 to 2021, PBMs are expected to save employers and consumers almost $2 trillion—or about 35 percent in savings—compared with drug expenditures made without pharmacy benefit management.
Prescription Drug Coverage Resources:
PBMs: A Critical Tool to Negotiate Lower Rx Prices
A fact sheet on the use of PBMs to provide affordable drug coverage to Texans and Texas businesses.
December 2016
Prescription drug spending is growing faster than any other part of the health care dollar (currently accounts for 24 percent of every $1 a consumer spends on health insurance). As the issue of skyrocketing pharmaceutical costs continues to be debated at the federal and state level, one critical tool that must be strengthened to keep prescription costs low is the use of pharmacy benefit managers (PBMs).
KEEPING PRESCRIPTION DRUGS AFFORDABLE: The Value of Pharmacy Benefit Managers (PBMs)
A resource guide on understanding how health plans and PBMs keep prescription drug coverage affordable.
September 2015
Health plans primarily use pharmacy benefit managers, or PBMs, as an efficient, effective way to manage prescription drug coverage and improve health outcomes. Some health plans maintain prescription drug management in-house, while others contract with PBMs outside of their organizations. PBMs help consumers and employers save on the cost of prescription drugs, while using clinically-based services to reduce medication errors and increase compliance with drug therapies.
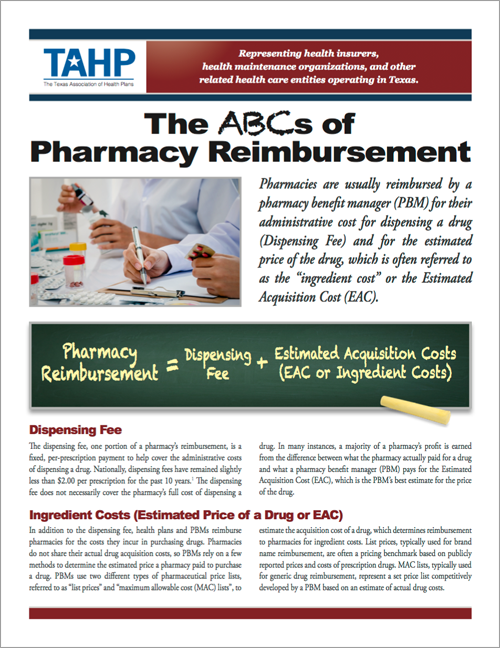
The ABCs of Pharmacy Reimbursement
A resource guide on understanding how pharmacies purchase prescription drugs and how they are reimbursed by health plans.
September 2015
Pharmacies are usually reimbursed by a pharmacy benefit manager (PBM) for their administrative cost for dispensing a drug (Dispensing Fee) and for the estimated price of the drug, which is often referred to as the “ingredient cost” or the Estimated Acquisition Cost (EAC).
Quick Facts on Independent Pharmacies
A fact sheet on how independent pharmacies are faring in Texas.
September 2015
In ongoing conversations about issues that impact pharmacy benefit managers (PBMs), legislators often discuss the welfare of independent pharmacies. The information in this brochure provides an overview of how independent pharmacies operate and how they are faring compared to large pharmacies that negotiate directly with PBMs.
PBM Regulations
A fact sheet on how PBMs are regulated.
September 2015
Pharmacy benefit managers (PBMs) are regulated by each state in which they operate and must comply with state licensing requirements. While it may vary from state to state, PBMs may be licensed and regulated as third-party administrators (TPAs) and/or utilization review agents (URAs) in appropriate states. In addition to licensing requirements, federal HIPAA and state privacy requirements also apply because PBMs act as business associates of their covered entity clients.
Keeping Prescription Drug Coverage Affordable: A Primer on PBMs
Power point presentation on prescription drug costs and coverage.
September 2015
Health plans and employers use PBMs as an efficient, effective way to manage prescription drug coverage and improve health outcomes. These third party administrators manage drug benefits, negotiate drug prices with manufacturers, negotiate rates and contracts with pharmacies, develops drug formularies, process and pays claims, and provide clinical drug management.