Texas Medicaid Rx Benefit
The Prescription for Medicaid Rx Savings: Carve It ALL In
From 2001 through 2011, Medicaid prescription drug costs had increased by 90 percent in Texas. This cost trend was no longer sustainable and without intervention, could have meant drastic reductions in the Medicaid program for consumers. In March 2012, prescription drugs were carved into Texas Medicaid managed care contracts. The decision was made by the 82nd Legislature not only for cost-savings, but also the need to improve access to care and quality. Since that time, Texas managed care organizations (MCOs), or Medicaid health plans, have made impressive strides in managing the Medicaid pharmacy benefit—saving millions in taxpayer dollars while improving the overall health of their clients.
Texas policymakers did the right thing in 2012 when they decided to allow the Medicaid health plans to manage the Medicaid Rx benefit. However, while handing off financial responsibility of the benefit to the plans, the State failed to give them the ability to fully manage the Rx drug benefit by requiring plans to use a single, uniform state Medicaid formulary instead of their own formularies. Every state’s Medicaid program has a preferred drug list (PDL). The PDL is a list of medications that a Medicaid client can receive without prior authorization. Texas’ PDL is currently managed by the Health and Human Services Commission’s Vendor Drug Program (VDP). Texas statute sunsets the State’s PDL in 2018 and would allow MCOs the opportunity to manage the PDL for the Medicaid clients they serve.
The Texas Association of Health Plans supports allowing MCOs to fully manage the pharmacy benefit in order to bring down costs and provide more timely access to clinically appropriate medications to Texans in the Medicaid program. Studies have shown that Texas Medicaid health plans could save taxpayers $100 million a year by fully managing the Rx benefit.
Medicaid Prescription Drug Resources:
The Prescription for a Healthier Medicaid Rx Program
A legislative guide to the scheduled transition of the Medicaid prescription drug benefit from the fee-for-service model to the managed care approach.
January 2017
Texas is a national leader in the use of managed care. Managed care has dramatically improved the lives, outcomes, and quality of care for Medicaid patients in Texas. Because of this success the Texas Legislature adopted the full expansion of managed care statewide in 2011, including the integration of the prescription drug benefit for Texans on Medicaid. Though the final step of this transition is already scheduled for August of 2018, the pharmaceutical industry is asking the Legislature to delay this transition to protect their profits and the current brand-name-heavy state system. TAHP supports allowing MCOs to fully manage the pharmacy benefit in order to bring down costs and provide more timely access to clinically appropriate medications to Texans in the Medicaid program.
Texas Medicaid Managed Care: Saving Dollars, Saving Lives
A fact sheet highlighting the success and outcomes of Medicaid managed care in Texas.
January 2017
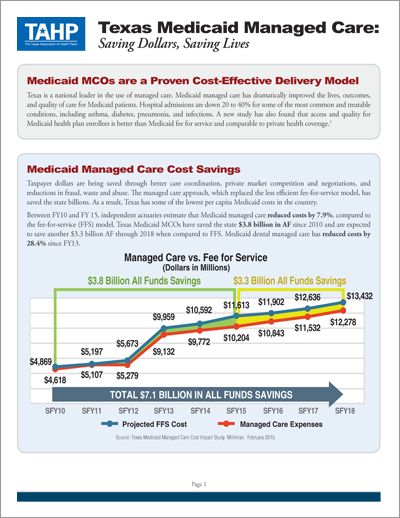
Texas is a national leader in the use of managed care. Medicaid managed care has dramatically improved the lives, outcomes, and quality of care for Medicaid patients. Hospital admissions are down 20 to 40% for some of the most common and treatable conditions, including asthma, diabetes, pneumonia, and infections. A new study has also found that access and quality for Medicaid health plan enrollees is better than Medicaid fee for service and comparable to private health coverage.
Benefits of Prescription Drug Management under Medicaid MCOs
A fact sheet highlighting efforts by MCOs to improve the costs and outcomes of the Medicaid prescription drug program.
April 2015
In March 2012, prescription drugs were carved into Texas Medicaid managed care contracts. The decision was made by the 82nd Legislature not only for the cost-savings, but also the need to improve access to care and quality. Since that time, Texas managed care organizations (MCOs) have made impressive strides in managing the Medicaid pharmacy benefit—saving millions in taxpayer dollars while improving the overall health of their clients.
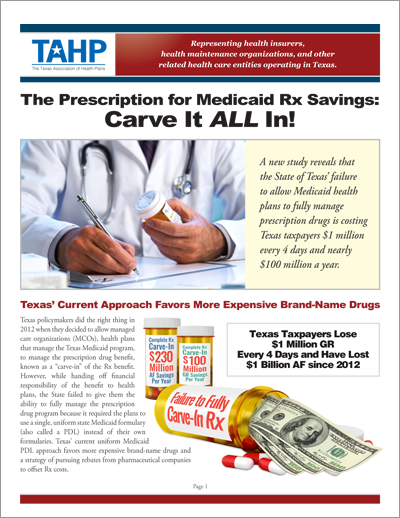
The Prescription for Medicaid Rx Savings: Carve It ALL In
A resource guide on how the Medicaid Rx benefit currently operates and opportunities for Texas to improve Rx quality and cost-effectiveness by fully carving the Rx benefit into managed care.
March 2016
Texas policymakers did the right thing in 2012 when they decided to allow managed care organizations (MCOs), health plans that manage the Texas Medicaid program, to manage the prescription drug benefit, known as a “carve-in” of the Rx benefit. However, while handing off financial responsibility of the benefit to health plans, the State failed to give them the ability to fully manage the prescription drug program.
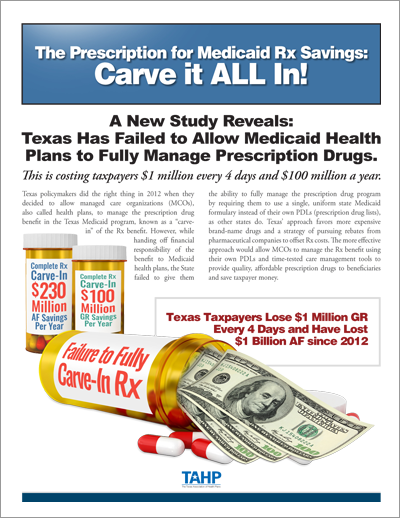
New Study Reveals: Texas Has Failed to Allow Medicaid Health Plans to Fully Manage Prescription Drugs
A fact sheet highlighting the findings from The Menges Group’s February 2016 study on the cost impact of allowing Medicaid health plans to fully manage the Rx benefit in Texas.
March 2016
A new study commissioned by TAHP finds that the incomplete carvein of the Medicaid prescription drug program is costing the State and taxpayers millions of dollars, and under this current structure, 21 states are out-performing Texas in managing drug costs with Rx costs that are 21% lower than the national average and 19% lower than Texas.
Assessment of Medicaid MCO Preferred Drug List Management Impacts
Study prepared by The Menges Group assessing the cost impact of allowing the Medicaid health plans to fully manage the Rx benefit in Texas.
February 2016
There are opportunities for Texas to achieve significant Medicaid prescription drug savings by allowing its managed care organizations (MCOs) to fully administer the Medicaid prescription drug program, including giving MCOs the flexibility (latitude) to manage the mix of drugs cost-effectively through their own preferred drug lists (PDL), also referred to as formularies.
Projected Impact of the Formulary Carve-In for Texas Medicaid and CHIP Programs
Study prepared by Milliman assessing the cost impact of allowing the Medicaid health plans to fully manage the Rx benefit in Texas.
February 2013
Milliman was engaged by the TAHP to evaluate the expected impact of moving from a single statewide formulary in the Texas Medicaid and CHIP programs to formularies specified by each managed care organization (MCO).
Presentation on the Assessment of Medicaid MCO Preferred Drug List Management Impacts
Presentation by The Menges Group highlighting the findings from their February 2016 study on the cost impact of allowing the Medicaid health plans to fully manage the Rx benefit in Texas.
March 2016
A study by The Menges Group for TAHP concluded that a policy change away from the uniform PDL administered by the VDP to a model where each MCO would manage its own PDL will yield significant savings to Texas’ taxpayers. These savings would be derived through drug mix management and would not involve any type of “cut” to Texas’ Medicaid program.