Texas Medicaid Managed Care
Protecting Texas Taxpayers from Fraud, Waste, and Abuse

Texas is a national leader in the use of managed care to increase access to care, manage costs, and improve health care quality in its Medicaid program. The managed care private-market approach drives innovation through flexibility and competition, reduces health care costs, and holds Medicaid health plans accountable for providing access to quality care.
Compared to the FFS model it replaced, the managed care approach has saved the state $4 billion over a six-year period. Over the next three years, it is expected to save an additional $3.3 billion. For the STAR program— Texas Medicaid’s largest managed care program, with 2.7 million consumers—costs grew only 2.2% from 2009 to 2013 while national health care costs grew nearly seven times as much, or 15%, over the same period of time.
Just as important, lives are being saved and improved due to integrated and coordinated care. Hospital admissions are down anywhere from 20 to nearly 40 percent for some of the most common—and preventable—conditions: asthma, diabetes, GI infections and more. Child “well visits” and childhood immunizations are surpassing national standards. Beneficiaries are also feeling more confident about the quality of their coverage and access to care. More than 80 percent of Texas families with children in managed care report an overall positive experience with their health plan and more than 90 percent report having access to their primary care provider.
Texas has saved dollars and lives through Medicaid managed care, and it has done so independently and innovatively—making the most of the managed care model. With greater flexibility, Texas can continue to achieve significant savings for taxpayers and healthier outcomes for the millions of Texans who depend on this critical program.
Quotes:
“Over the past 20 years managed care has revolutionized the delivery of Medicaid health care services in Texas.” – Sellers Dorsey, Medicaid Managed Care in Texas, February 2015
“Texas has been very innovative in our policies to ensure Medicaid services are provided in a cost-effective manner through managed care.” – Governor Greg Abbott, September 29, 2015 letter to the federal Centers for Medicare and Medicaid Services
Medicaid Managed Care Resources:
Texas Medicaid Managed Care: Protecting Texas Taxpayers from Fraud, Waste, and Abuse (FWA)
Background on Texas managed care plans’ efforts to reduce fraud, waste and abuse in Medicaid.
September 2016
MCOs are successfully focusing their efforts on preventing FWA, reducing inappropriate payments, and finding real-time results and methods to transition away from the pay-and-chase environment common under the former fee-for-service model (FFS).
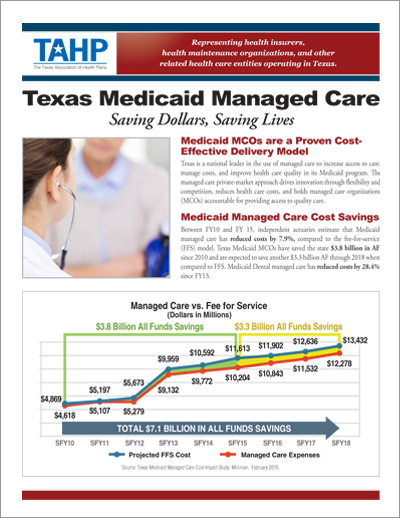
Texas Medicaid Managed Care: Saving Dollars, Saving Lives
A fact sheet highlighting the success and outcomes of Medicaid managed care in Texas.
October 2015
Between FY10 and FY 15, independent actuaries estimate that Medicaid managed care has reduced costs by 7.9%, compared to the fee-for-service (FFS) model. Texas Medicaid MCOs have saved the state $3.8 billion in AF since 2010 and are expected to save another $3.3 billion AF through 2018 when compared to FFS. Medicaid Dental managed care has reduced costs by 28.4% since FY13.
TAHP Testimony to Senate Health and Human Services Committee
Presentation on Texas Medicaid managed care efforts to reduce fraud, waste, and abuse.
September 2016
This presentation shows how Medicaid MCOs are transforming their efforts to focus on prevention, reducing inappropriate payment, and finding real-time results and methods to transition from a pay and chase environment.
Medicaid Managed Care: A Fiscally Responsible Pathway to a Healthier Texas
A resource guide on how Medicaid managed care operates in Texas.
October 2015
Texas is a national leader in the use of managed care to increase access to care, manage costs, and improve health care quality in its Medicaid program. The managed care private market approach drives innovation through flexibility and competition, reduces health care costs and holds managed care organizations (MCOs) accountable for providing access to quality care.
Medicaid Managed Care in Texas: A Review of Access to Services, Quality of Care, and Cost Effectiveness
Study prepared by national research firm Sellers Dorsey evaluating access to care, quality of care, and the cost-effectiveness of the Texas Medicaid managed care program.
February 2015
Over the years numerous studies and evaluations have concluded that the Texas Medicaid managed care program was indeed meeting its promise to improve access, reduce cost, and improve quality of care. Expanding Medicaid managed care has been a key Texas strategy for reforming its Medicaid program. Over the last 20 years the population in Medicaid managed care has increased from 58,000 members to over 3 million members.
Texas Medicaid Managed Care Cost Impact Study
Study prepared by national research firm Milliman evaluating the cost impact of the managed care model on the Texas Medicaid program.
February 2015
This study reveals that from SFY2010 to SFY2015 costs under the Medicaid Managed Care program are significantly less as compared to estimated expenditures on a fee-for-service structure. Savings of nearly $3.8 billion, or 7.9% have been realized during this six year period.