Texas Medicaid Managed Care Networks
Ensuring Access to Quality Care

Texas is a national leader in the use of managed care to increase access to care, manage costs, and improve health quality in its Medicaid and CHIP programs. Texas managed care organizations (MCOs)—or the health plans that contract with the State to manage Medicaid—establish provider networks to ensure their members have guaranteed access to quality health care providers. Many states, including Texas, have enacted network adequacy standards to ensure that Medicaid health plans are providing access to the right kind of care for their members at the right time and the right location. “Network adequacy” refers to a health plan’s ability to deliver plan benefits by providing reasonable access to a sufficient number of contracted providers. Texas’ MCOs have effectively improved access to and quality of care for Texas Medicaid beneficiaries while containing costs for the state. Additionally, Texas MCOs have implemented innovative solutions not possible under the traditional fee-for-service model (FFS) to improve access to care beyond network adequacy requirements.
Medicaid Managed Care Networks Resources:
Medicaid Managed Care: Ensuring Access to Quality Care
A resource guide on how Texas Medicaid health plans ensure their enrollees have access to the right care, at the right time, in the right place, and how the Health and Human Services Commission (HHSC) monitors network adequacy.
December 2015
Access to care is an essential part of any health care delivery system, and the Texas Medicaid program is no exception. Ensuring that Medicaid consumers have access to the right kind of care for their needs at the right time leads to improved health outcomes for Medicaid patients and lower costs for Texas taxpayers.
TAHP Presentation to SB 760 Workgroup on Network Adequacy
Presentation to HHSC and SB 760 Workgroup on Medicaid MCOs’ efforts to ensure access to care.
June 2016
In this presentation TAHP recommends that Texas needs a comprehensive assessment on levels of Medicaid provider participation, and while distance and wait time standards are common and useful ways to assess network adequacy standards, the state should be cautious about over-reliance on these standards alone.
TAHP Presentation on Medicaid MCO Network Adequacy
Presentation and overview on Texas Medicaid MCO network adequacy standards and MCOs’ efforts to ensure access to care and improve outcomes.
June 2016
In this presentation TAHP indicates there are significant opportunities through a partnership between HHSC, the MCOs, and provider groups/associations working together to improve provider education and outreach, and to make education/training available to providers for specific Medicaid populations.
HHSC Presentation to SB 760 Workgroup on Network Adequacy
HHSC presentation on network adequacy requirements, comparison to other states’ requirements, and MCO efforts to ensure access to care in the Texas Medicaid program.
June 2016
In this comprehensive presentation HHSC discusses and recommends ways to strengthen Medicaid managed care organization (MCO) provider networks, including: provider access standards, provider directories, and expedited credentialing.
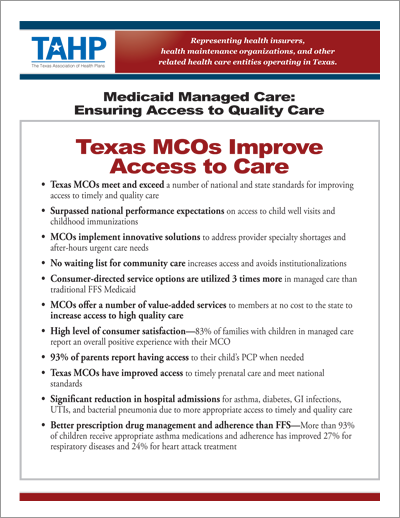
Texas Medicaid MCO’s Improve Access to Care
A resource guide on MCO efforts to improve access to care for the Texas Medicaid program.
April 2015
Despite the challenges of Medicaid, managed care has proven to be an effective tool for improving access to care in Texas, and Medicaid managed care organizations (MCOs) continue to implement innovative solutions to increase access to care not possible under the old fee-for-service (FFS) model.